What is Neurogenic Bladder?
We are back to answer another one of those "wait, neurogenic what?" questions! Whether you have been Googling your symptoms or were diagnosed by a medical provider, you may be wondering “what is neurogenic bladder?”
In this blog post we explain what neurogenic bladder syndrome is, how additional factors can impact our bladder, the common diagnoses associated with neurogenic bladder, and how pelvic floor physical therapy can help you manage your neurogenic bladder.
What does neurogenic bladder mean?
Neurogenic bladder occurs when you bladder control is impaired due to a brain, spinal cord, or nerve problem/injury that impacts the nerves that control the bladder. Neurogenic bladder is also commonly referred to as Neurogenic Lower Urinary Tract Dysfunction (NLUTD).
Let’s talk anatomy.
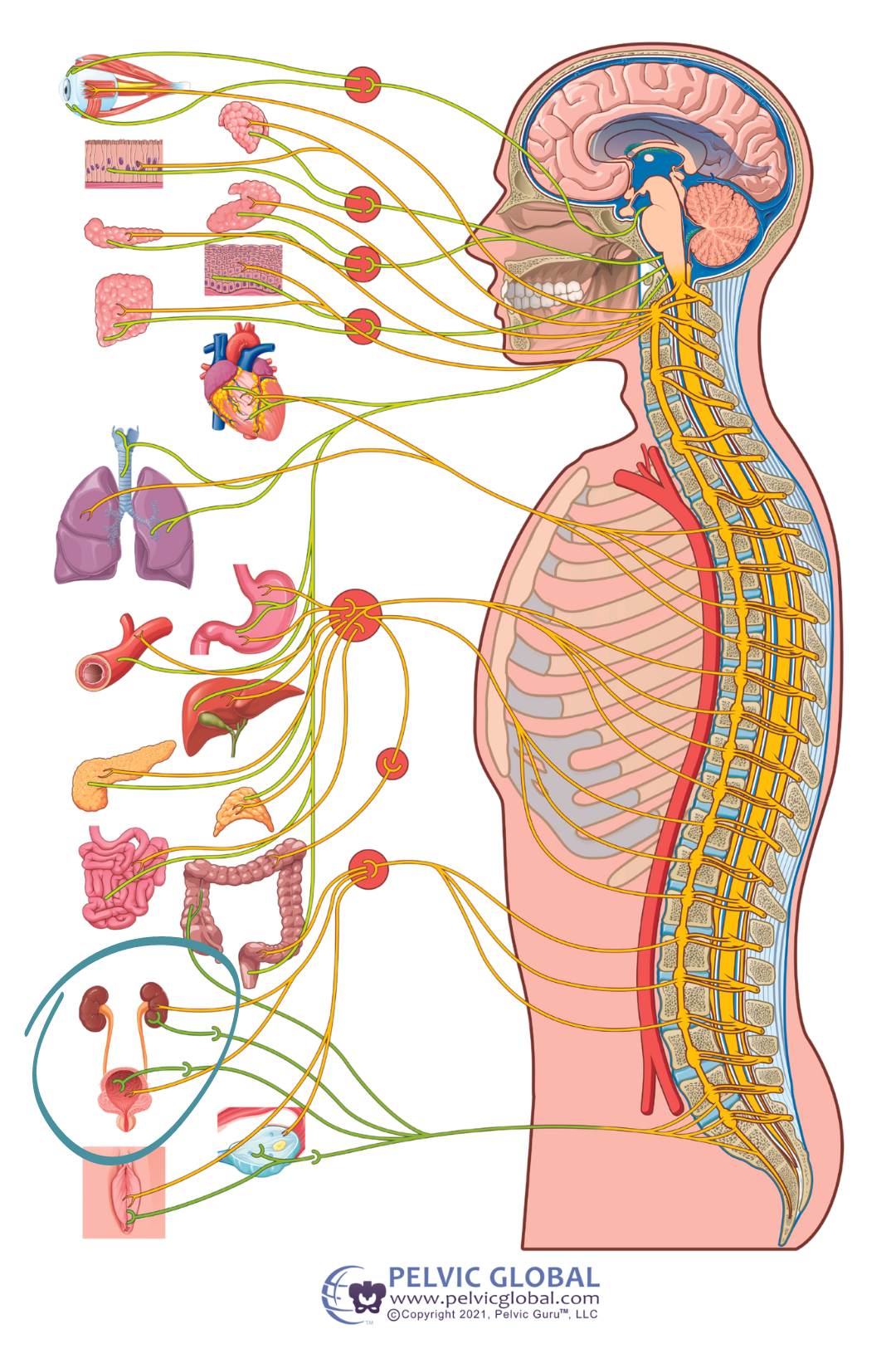
The bladder functions through a series of neural pathways and reflexes under a combination of voluntary and involuntary control. The bladder system communicates with the brain via our peripheral nerves and spinal cord, as well as with our pelvic floor muscles to coordinate bladder filling, storage, and emptying.
Our bladder has the capacity to hold between 400-600 mL of fluid (or about 1.5 to 2.5 cups) and when we pee, typically 300-500 mL (or 1.25 to 2 cups) comes out.
As the bladder starts to fill, the detrusor muscle that wraps around the bladder (pictured below) will typically remain relaxed or inactive. At the same time, the pelvic floor muscles, which provide bottom-up support to the bladder, are active to help keep the urethra stay closed while the bladder stores urine.
When the bladder is nearly full, the detrusor muscle will stretch and the nerves from the detrusor muscle will send messages to the brain via the spinal cord to signal the need or urge to head to the bathroom to empty.
When ready to empty, the brain sends messages down the spinal cord to the bladder to signal the detrusor muscle to contract around the bladder. This will create an increase in pressure in the bladder which is stronger than the pressure of the urethral sphincter muscles and urine will start to flow.
With this cycle of the bladder in mind,
if there is an injury or dysfunction anywhere along these pathways, such as the nerve connections between the brain and the detrusor muscle of the bladder,
there likely can be an impact on the body’s ability to move, store, or empty urine.

What are the ways neurogenic bladder or NLUTD can result in bladder dysfunction?
Overactive
With an overactive neurogenic bladder, the nerves send signals to the bladder too frequently, resulting in bladder spasms and possibly the feeling of bladder fullness when the bladder may only be partially full. This can result in a strong, sudden urge to urinate, a frequent urge to urinate, and/or leakage of urine while trying to get to the bathroom on time.
Underactive
An underactive bladder can be due to an underactive detrusor muscle where this bladder muscle may not contract when needed or may have a weak contraction. When the contraction is weak, the pressure in the bladder may not be strong enough to overcome the pressure of the urethral sphincter muscles which will make it hard to let urine out. This can result in urinary retention, a slow or dribbling stream, and/or the need to strain to empty the bladder.
Combination of overactive and underactive
Over- and under-activity can occur simultaneously for some individuals with neurogenic bladder, possibly resulting in both urinary leakage and retention. This can look like frequent bladder spasms resulting in that sudden urge to go, however weak contractions of the detrusor muscle decreases the bladder’s ability to empty.
Detrusor sphincter dyssynergia (DSD)
DSD can occur when an overactive bladder may be working against closed and/or tight sphincters. When this is occurring, the detrusor muscle will contract to try to empty the bladder, however the sphincter muscles that provide bottom-up support to the bladder at the urethra may remain closed. This lack of coordination between the bladder and sphincters can result in urinary retention.
What do neurogenic bladder symptoms look like?
Our patients that suffer with neurogenic bladder often report:
- Urinary Incontinence (leakage of urine) associated with urgency (trying to get to the bathroom on time) or stress on the system (cough, laugh, sneeze, or with activity like standing up or walking)
- Urinary urgency or frequency (a strong or frequent need to go, including urinating more than every 2-4 hours during waking hours or 8 times daily, or more than 0-1 times at nighttime)
- Urinary retention (difficulty emptying the bladder)
- Typically, there is a small amount of urine left in the bladder after emptying of ~50-100 milliliters. You may have urinary retention and/or difficulty emptying your bladder if a medical professional has stated you have an ‘elevated’ or a ‘high PVR’ (PVR - post-void residual), typically >100 milliliters.
- Difficulty starting urine stream or weak urinary stream (straining to start a urine stream or to empty at the end of toileting is a common symptom reported)
Bladder symptoms can be impacted by additional factors, such as:
- Functional mobility- Are you able to safely get to the bathroom on time to empty?
- Arm, trunk, and lower body mobility and dexterity- Any difficulties or discomfort with removing clothing/pants, transferring to the toilet, or maintaining a seated or standing position while trying to empty your bladder?
- Schedule constraints- How much time do you have to complete your bladder routine? This can especially be important for folks who complete clean intermittent catheterization.
- Dietary changes- What does fluid intake currently look like? This will impact the concentration or dilution of the urine and its impact on the lining of the bladder.
- Fatigue- Are symptoms of fatigue impacting your ability to get to the bathroom on time and safely?
- Medication side effects- Certain medications may have side effects that impact urinary retention, urgency, and frequency
- Comorbid conditions- other diagnoses such as Diabetes or even chronic constipation can impact bladder function and control
What diagnoses are associated with neurogenic bladder?
Neurogenic bladder symptoms can occur due to a number of neurological conditions, including but not limited to:
- Traumatic and nontraumatic brain injury
- Multiple Sclerosis
- Parkinson’s Disease
- Spinal Cord Injury
- Cerebral Palsy
- Spina Bifida
In addition to the listed diagnoses above, we at Pelvic Pride work with individuals navigating other neurologic conditions, including post-concussion syndrome, tethered cord, transverse myelitis, and Guillain-Barré syndrome (GBS), to name a few. Please feel free to give us a call for a free phone screening to learn if pelvic therapy is the right fit for you!
So how can pelvic therapy help with neurogenic bladder?
Most folks may not realize pelvic health therapy can be helpful for the management of neurogenic bladder symptoms! Maybe you’re still experiencing difficulty emptying your bladder after a CVA or traumatic brain injury, or noticing some unwanted leakage of bladder with a sneeze or during exercise or sexual activity.
Your pelvic health therapist should focus on education regarding the root cause of your symptoms and treatment to best support your symptoms with a goal to maximize any intact sensation or motor function. This can include strategies for:
- Bladder routine support
- Fall risk assessment
- Caregiver education and training
- Breathing exercises
- Lumbo-pelvic mobility & strengthening
- Pelvic floor muscle coordination training
- Soft tissue mobilization, or hands-on external or internal pelvic floor work
What are the results that someone can expect from pelvic PT?
Great question! Although a pelvic-neuro pelvic health therapist cannot revert, alter, or prevent any pathological nervous system changes due to a progressive or non-progressive neurological condition, our goal is to find treatment techniques and strategies that best support your bladder symptoms, help you improve your quality of life, and gain or maintain control over your bladder!
Common results of pelvic PT include:
- Improved daily bladder habits and routine to address urinary symptoms that can be getting in the way of your daily activities, such as getting to work on time, exercising without leakage symptoms, and even sexual function and health
- Decreased urinary leakage that may occur with daily tasks including functional mobility like transfers, walking, or trying to get to the bathroom on time
- Improved bladder frequency, urgency, and/or emptying ability
- Improved awareness and coordination of the lumbo-pelvic musculature, including pelvic floor, abdominals, spinal, and hip muscles, dependent on intact innervation of these muscles
- Improved scar tissue mobility and sensitivity if present following a traumatic event
- Improved overall knowledge of the anatomy and function of the nervous system (brain, spinal cord, and nerves) and connection with the bladder and pelvic floor musculature
Where to find treatment in Maryland
At Pelvic Pride Physical Therapy & Wellness, Dr. Marlena specializes in the treatment of neuro pelvic floor conditions, so you are in the right place! We are conveniently located in the Federal Hill neighborhood in Baltimore MD. Fill out our contact form & our Patient Care Specialist will reach out to you ASAP!
Next on Your Reading List
Love our content? Let's stay connected!
Subscribe to our newsletter for personalized updates when new blog posts are dropped.